January 25, 2022
Survey Findings of The AXA Study of Mind Health and Wellbeing in 2022
It has been two years since the World Health Organization (WHO) declared COVID-19 to be a pandemic. Despite often harsh preventative measures and the remarkably swift development and rollout of new vaccines, the disease remains with us and continues to take a heavy toll. As such, it’s a key factor in AXA’s Mind Health Study, with mental wellbeing considered in almost every country to be the second-biggest casualty of the pandemic behind the economy.
9 minutes
Being mind-healthy: Why good mind health is key to our social and financial wellbeing
This article is part of the AXA Study of Mind Health and Wellbeing in Europe and Asia 2022.
ACCESS THE FULL STUDYAgainst the grim backdrop of the pandemic, there are some positive elements. According to our study, 35% of people claim the pandemic has made them more mentally resilient, improving their ability to face big challenges. It has also pushed mind health issues to the fore. All too often, in the past, stigma and social taboos have prevented people from admitting they need help. COVID-19 has gone some way toward changing that. The unprecedented, global nature of the pandemic means everybody has been affected by it to some degree and can relate to its psychological pressures. Aside from the fear of catching the disease and the trauma that may bring are the many ways it has disrupted Survey findings our daily lives – adapting to working from home, temporary or permanent unemployment, lost income, school and university closures, restrictions on social interaction. As a result, there is a growing understanding of the need to discuss mental health and a greater empathy toward those who are struggling to cope. Our study shows that parents want to involve their children in this conversation and to explore ways of supporting the mind health of future generations.
The information gathered here has helped us to construct the AXA Mind Health Index, a measuring tool used to assess the current mental wellbeing of individuals, communities and countries, pinpointing areas of weakness and outlining ways these can be addressed (visit our page on the AXA Mind Health Index).
Most people are just getting by
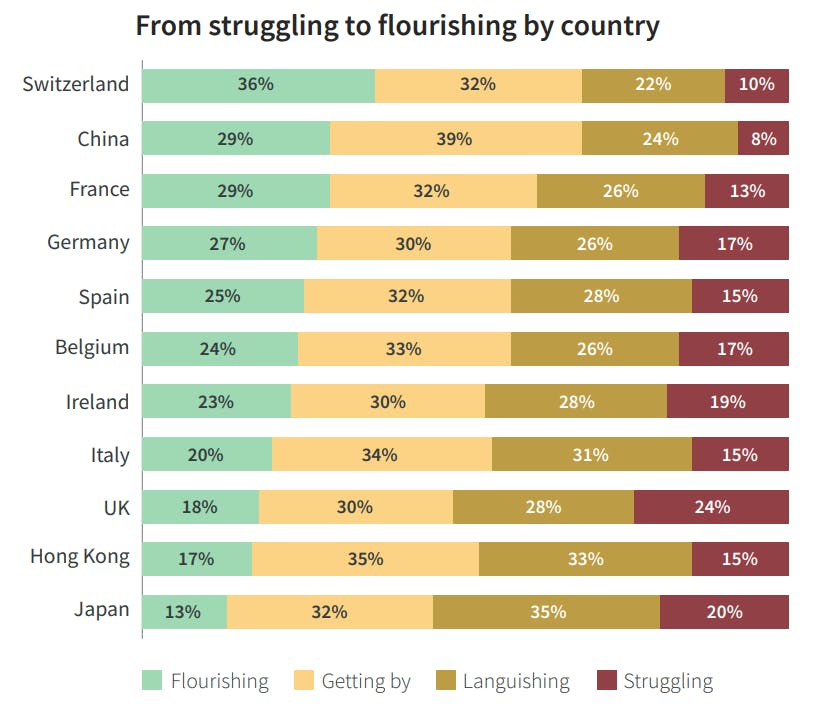
AXA commissioned Ipsos to poll 11,000 people aged between 18 and 75 in 11 European and Asian countries and territories. These included France, the UK, Germany, Spain, Italy, Ireland, Belgium, Switzerland, China[1] , Hong Kong and Japan. Depending on their responses, people were ranked in four mind health bands, from flourishing at the top, through getting by and languishing to struggling at the bottom.
Our study found the largest proportion of people were just getting by, counting for one-third of those questioned. These were people who had some sense of wellbeing, but not enough to say they were flourishing. Less than a quarter hit that flourishing pinnacle. This is true across most individual countries apart from Switzerland where an impressive 36% of people were classed as flourishing
Joy and stress
From a range of factors that might bring joy or stress, from the pandemic through job security, finances, social life and family, none in our study was either fully positive or negative. The pandemic, with its consequent lockdowns and the impact on the economic and political situation, was the biggest source of stress. Over half of respondents cited its negative impact. Views of financial security and social lives were predominantly negative, but by a much smaller margin. Perhaps more surprisingly, given the restrictions imposed by governments during much of the health crisis, there were several areas where joy outstripped stress. Family life was the main beneficiary while people were also buoyed by their new-found resilience and coping skills. Many found pleasure in working from home and in improving their physical health.
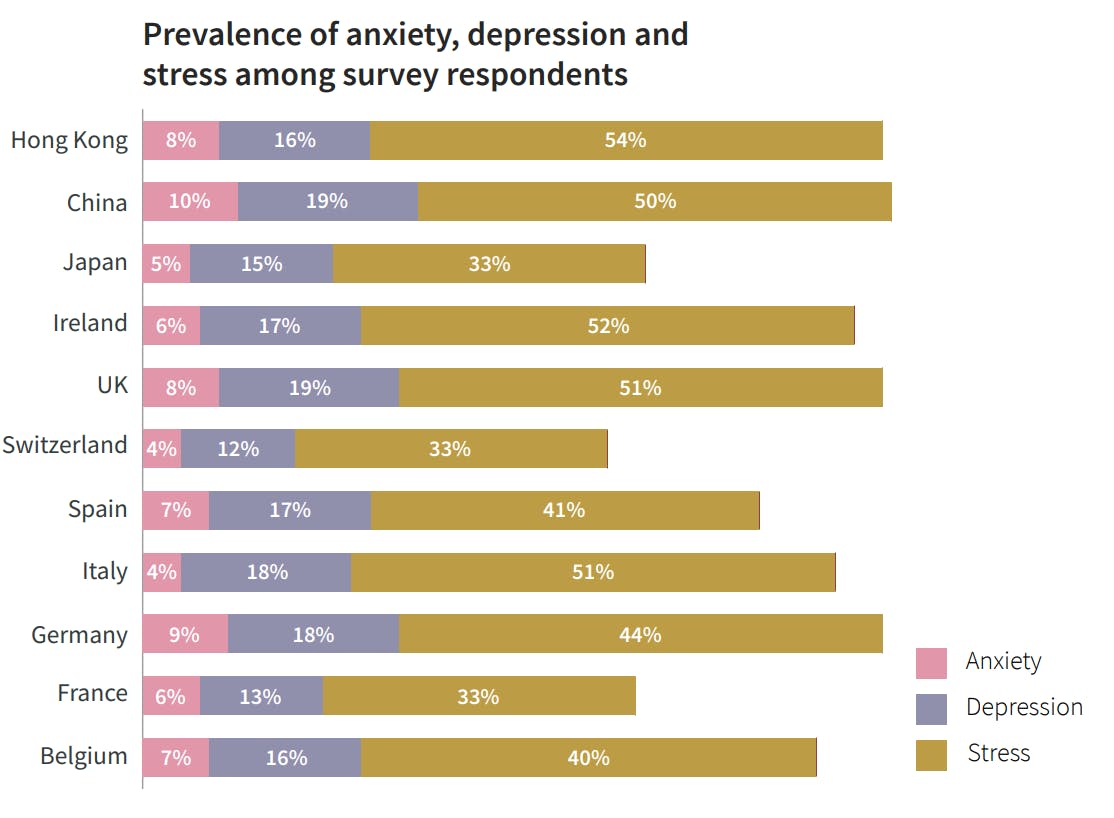
Even with these sometimes positive aspects, stress levels remained troublingly high in several countries or territories. In Hong Kong, Ireland, Italy and the UK, over half the study group said they were experiencing stress. Though stress isn’t classed as a mental illness, it can be a step along the road to anxiety and depression. Stress usually stems from an identifiable source – perhaps job insecurity or financial worries – and will disappear if these pressures are removed. Anxiety and depression are more deep-rooted and may not be helped by the removal of external pressure. Depression is less prevalent than stress, but the numbers are still alarmingly high. China and the UK head the list for depression, where just under one-fifth of those surveyed were affected by it. Rates for Italy and Germany were not far behind.
Over half of those surveyed said they had experienced high levels of stress in the last year, rating it above six on a scale of zero to 10. Less than half said they had felt happy, experienced joy or felt they were able to develop as a person.
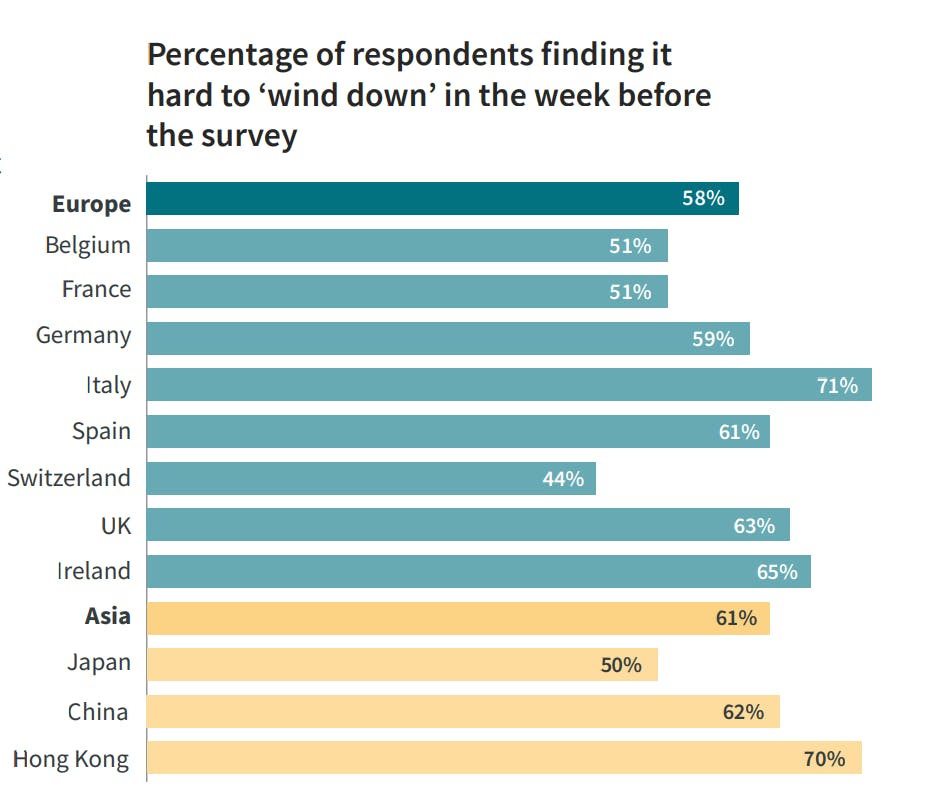
Narrowing it down to how they fared in the week before being interviewed, over half said they experienced symptoms of depression and anxiety, felt low or agitated and found it hard to wind down. These symptoms were above average in Italy, Ireland and the UK. Asian countries were found to be under slightly more stress than Europe, particularly in Hong Kong.
Across our study, those optimistic about the future outweighed pessimists by 43% to 32%. The number of optimists was above average in Switzerland, Ireland and Spain.
Happy or unhappy at work
The workplace plays an important role in any assessment of community‑wide mental health, being a possible source of problems but also potentially a useful tool for promoting wellbeing. It benefits both employees and employers if people feel supported at work.
When workers feel unduly stressed, inefficiency and absenteeism are bound to rise, potentially affecting a company’s financial performance. Even in a low-stress workplace, it makes sense for businesses to help employees deal with issues they may face outside.
The WHO has highlighted the importance of monitoring and minimizing stress at work, particularly in periods when businesses are transforming. Workers who are stressed, it believes, are more likely to be unhealthy, poorly motivated, less productive and less safe at work. Moreover, their organizations are less likely to be successful in a competitive market[2] .
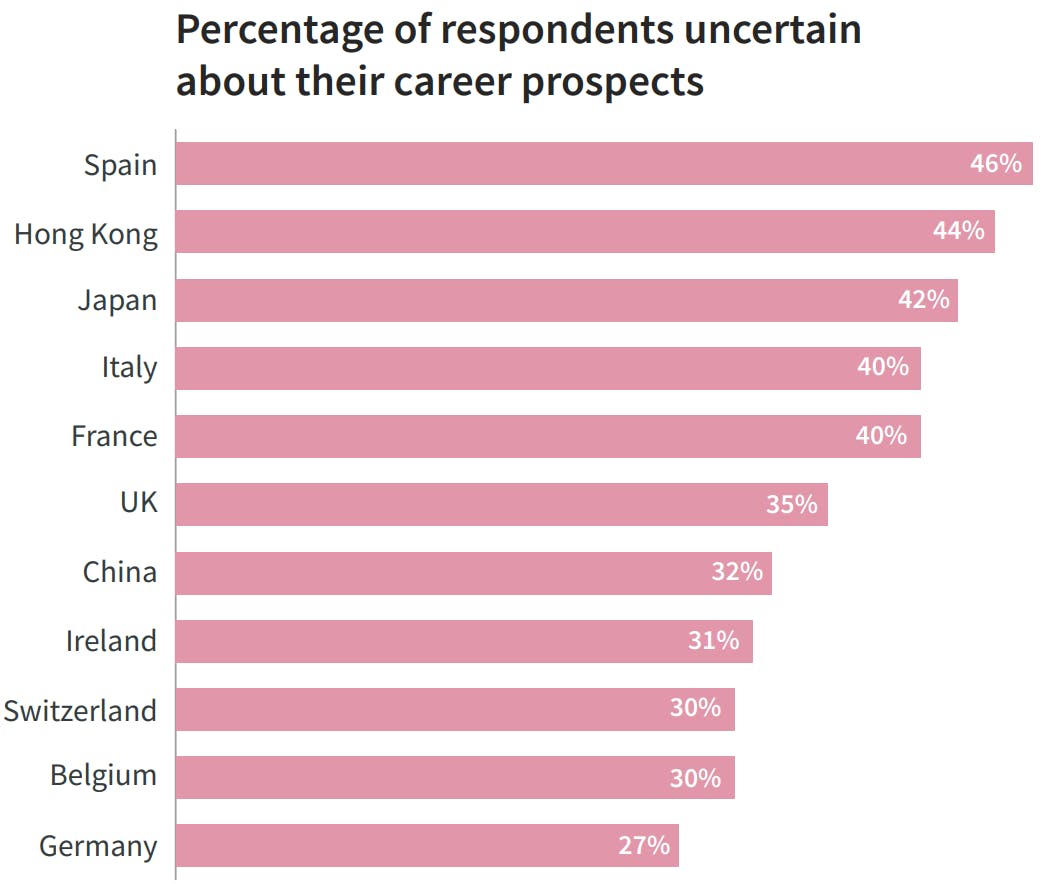
Our study results suggest the approach to promoting mind health in the workplace is patchy at best. A high number of people admit to feeling uncertain about their career prospects. This was most pronounced in Spain and Hong Kong where almost half said they were insecure at work. Recent history may play a part in this. Spain was one of Europe’s hardest hit countries in the banking crisis of 2008, when unemployment rose sharply. By contrast Germany, the EU’s largest economy, suffered fewer economic problems and just over a quarter of Germans surveyed said their career prospects were uncertain, the lowest of all the countries or territories included in our poll.
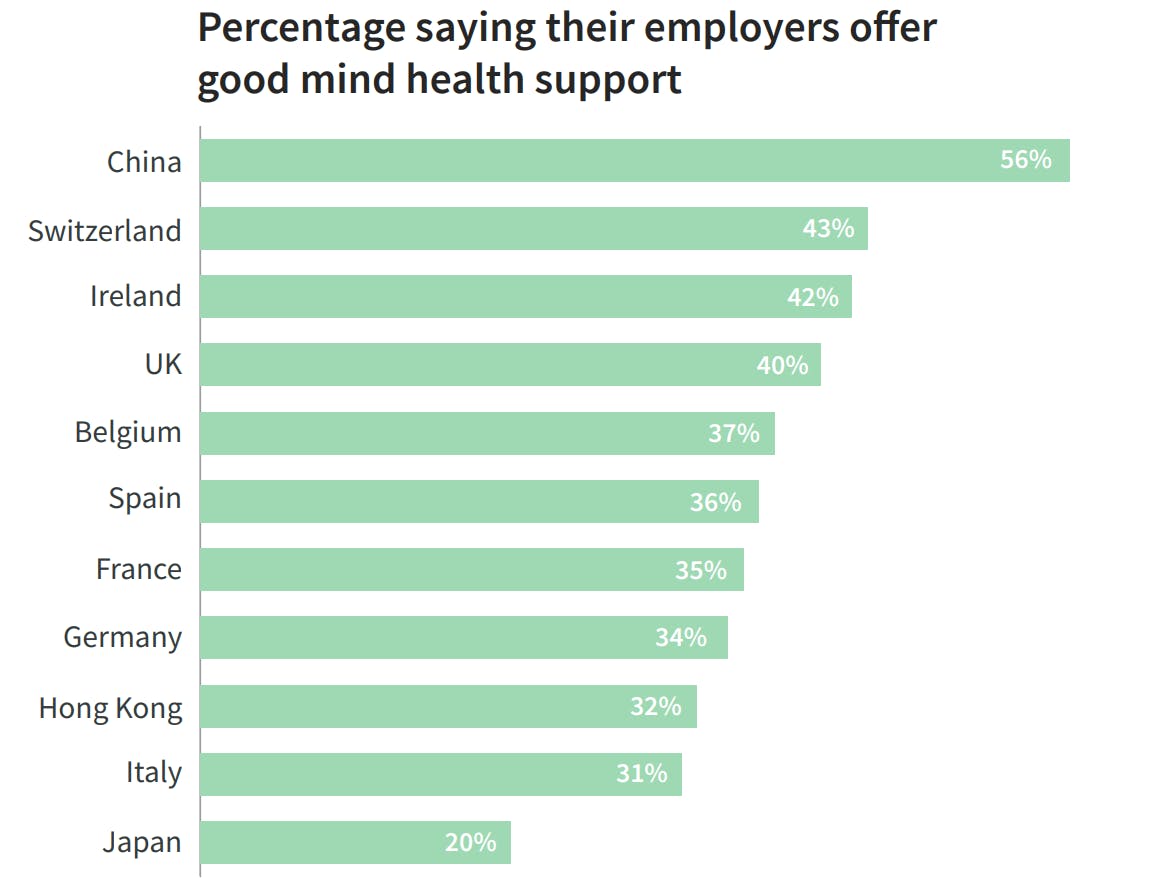
Overall, despite relatively high levels of depression, Chinese employees said they were more content at work than people elsewhere. They scored more highly than any other country for having a positive workplace culture, were more likely to have a good work-life balance and felt better supported by employers. Those working for employers who were supportive of mind health were twice as likely to flourish as those who didn’t.
Fewer in Hong Kong and Japan claimed to have the right work-life balance than anywhere else apart from Germany, and they had the smallest number of people who said their workplace culture was positive.
Mind the gender gap
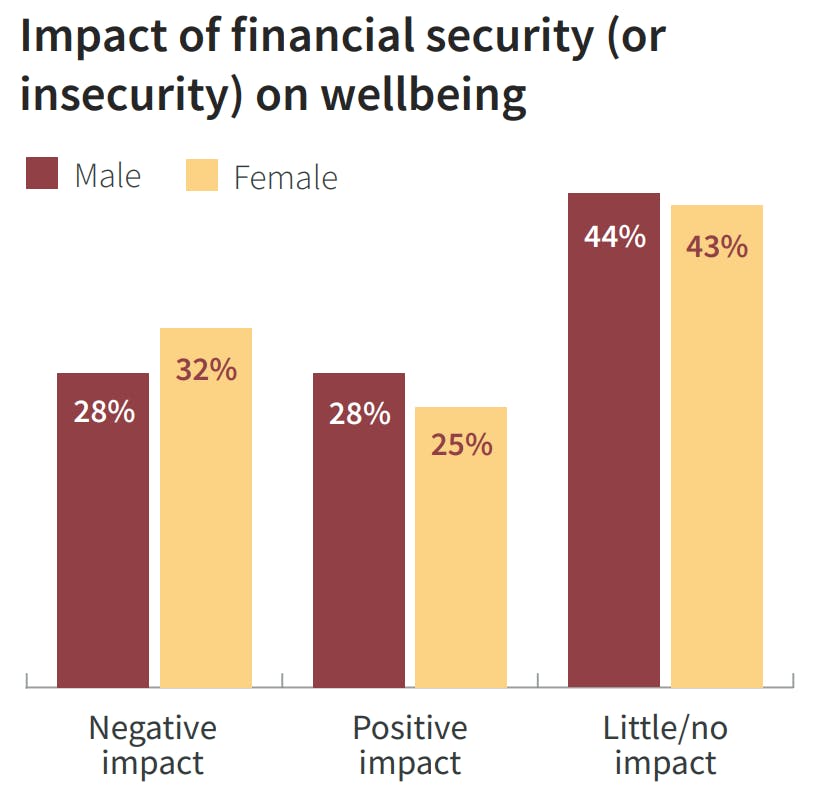
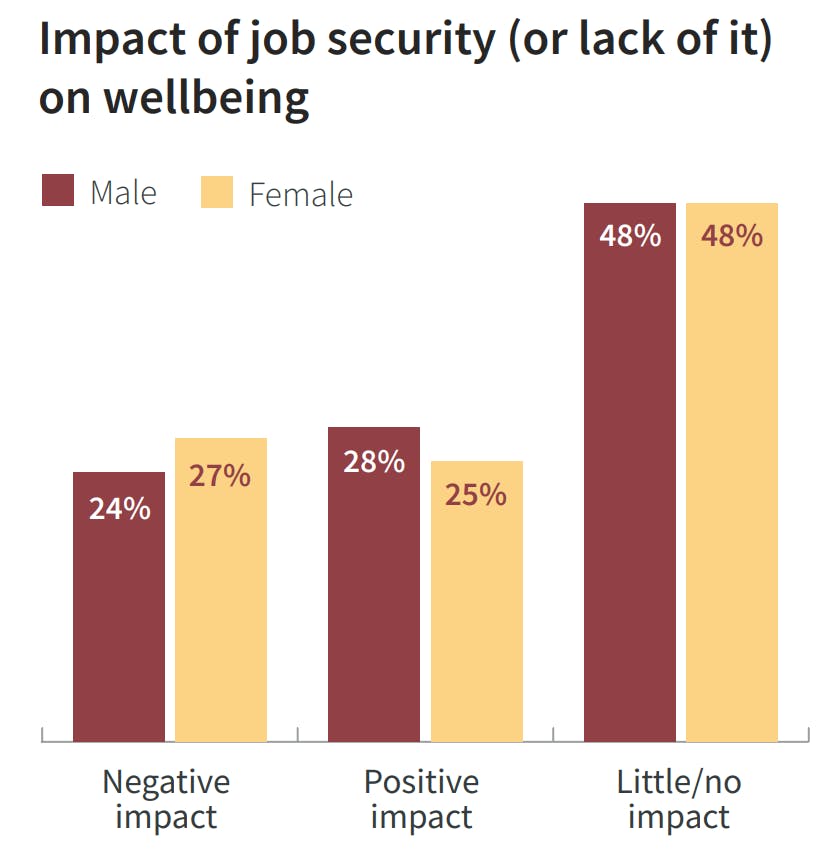
Men fared better than women across most of our study. Even where results were largely positive, women lagged behind men. This is often because women tend to have more financial concerns than men and are more likely to be in insecure or low-paid jobs.
As such, job and income security has been more of an issue for women than men. More women lost their jobs or were put on reduced hours because of the pandemic. Those in work earn less on average – just 77 cents to every dollar paid to a man[3].
More typically, women work in sectors hardest hit by the pandemic, including schools, healthcare and hospitality.
Though a majority of men and women felt family life had been either a positive or at least neutral contributor to their wellbeing in the last year, within the minority who said it was negative, women outstripped men by a 30% margin. As highlighted in a previous AXA report[4] , this may be due to women being more likely to take responsibility during the pandemic for their families’ wellbeing, juggling homeschooling, work and domestic chores.
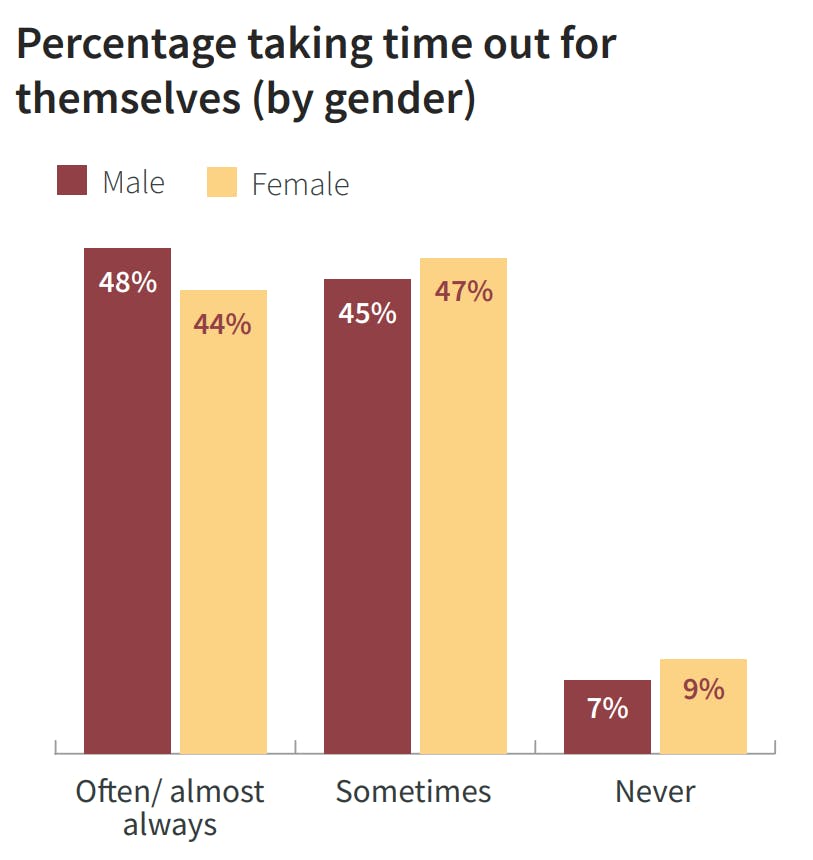
All this has a clear impact on the ability of women to take care of their own mental wellbeing. They have less me-time than men, do less physical exercise and are more likely to dwell on the negative when things go wrong, making it harder for them to recover from mental health pressures.
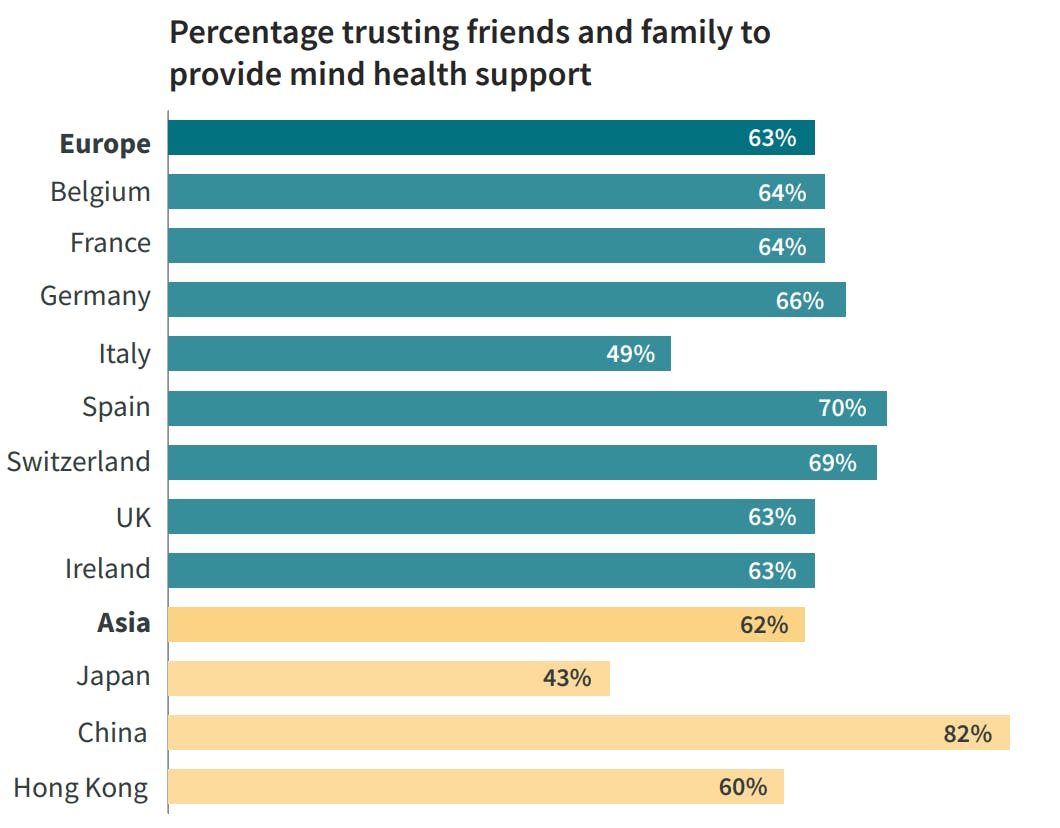
Adding to these issues is a lack of faith among women in the ability of public health services to treat mental illnesses. Perhaps for this reason, women are more likely to shun healthcare professionals and turn instead to close friends and relatives in times of stress.
These constraints may indicate why, overall, women showed less self-acceptance than men, and less faith in their own abilities – both important elements for people to flourish.
The relative difference between how men and women responded in our survey doesn’t necessarily mean men don’t experience severe distress. Research has shown that, while women are more likely to report symptoms of anxiety and depression, men have higher overall rates of suicide[5] . This may be because men don’t disclose their mental health issues in the same way as women. A report in the American Journal of Men’s Health suggests inadequate surveys into men’s experiences and a subconscious tendency for health professionals to overlook male distress may lead to underestimates of depression and anxiety among men[6] .
Youngsters seen as most affected by pandemic
In Europe, children and teenagers were identified as the most affected mentally by the pandemic.
Under 18s weren’t surveyed so this response came from older age groups, suggesting an awareness by older people of the impact of the pandemic on the younger generation, identifying an area where action now would support better mind health in the future. There were a couple of exceptions, with France and Switzerland saying 19 to 29-year-olds were hardest hit, while Belgium and all three Asian countries and territories reckoned every age group suffered equally. The importance of supporting younger generations is acknowledged by parents, with the majority in all countries believing mental health should be discussed with children.
Perhaps most interestingly, the people who came through as being most affected by the pandemic – rather than those who were perceived to be – were in the 25 to 34 -year age group.
Dealing with mental illness
The quality of healthcare is critical to the future happiness of those who become mentally ill. Those who have been diagnosed with illnesses in the past are more likely to experience ill-health again in future.
Of those surveyed, just over a quarter said they were experiencing mental health problems or had experienced them in the past. The most common illnesses were depression, anxiety, phobias or post -traumatic stress disorder (PTSD) – to a lesser degree, there were also eating disorders, substance abuse, obsessive compulsive disorders, schizophrenia and related bipolar illnesses.
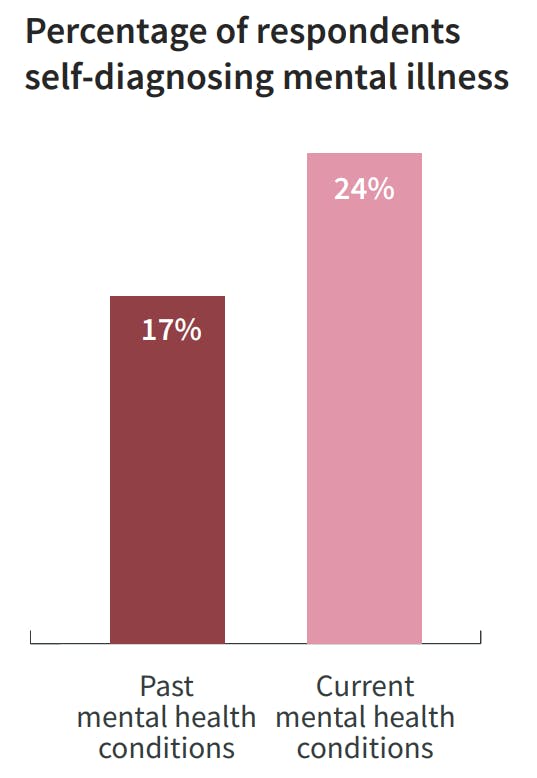
While mental illnesses are still mainly diagnosed by healthcare professionals, there is some indication of a shift toward self-diagnosis via the internet.
Those who are currently being treated showed a slightly higher proportion of self-diagnosis than those who had been ill in the past. Between the two groups there was a corresponding decline in the number of mental illnesses diagnosed by General Practitioners (GPs) or family doctors. This could be at least partly due to restrictions on in-person medical visits during the pandemic or because people were more nervous about going to consulting rooms. Self-diagnosis of current illnesses was strongest in China, Hong Kong and Italy, where it outstripped diagnosis by psychologists, psychiatrists and GPs.
The quality of public healthcare could be a factor too. Even countries or territories with well-funded and efficient services aren’t always considered to be proficient at tackling mental illness. Only 38% of those surveyed believed their local health service was up to the mark. China and Switzerland were well above average at 65% and 58%, respectively. The Swiss and Chinese were among those most likely to depend on family and friends if they became ill.
The confidence Chinese people have in their public health services appears to be at odds with their willingness to self diagnose. This may be because of the relatively low number of mental healthcare professionals in China. In 2015, China’s State Council launched an ambitious plan to double the number of psychiatrists to 40,000 by 2020. This would still represent only 28 psychiatrists for every 1 million people. Social prejudice may also be a reason so many seek the anonymity of the internet – though half of those polled in our study in China said they believed stigma had declined during the pandemic.
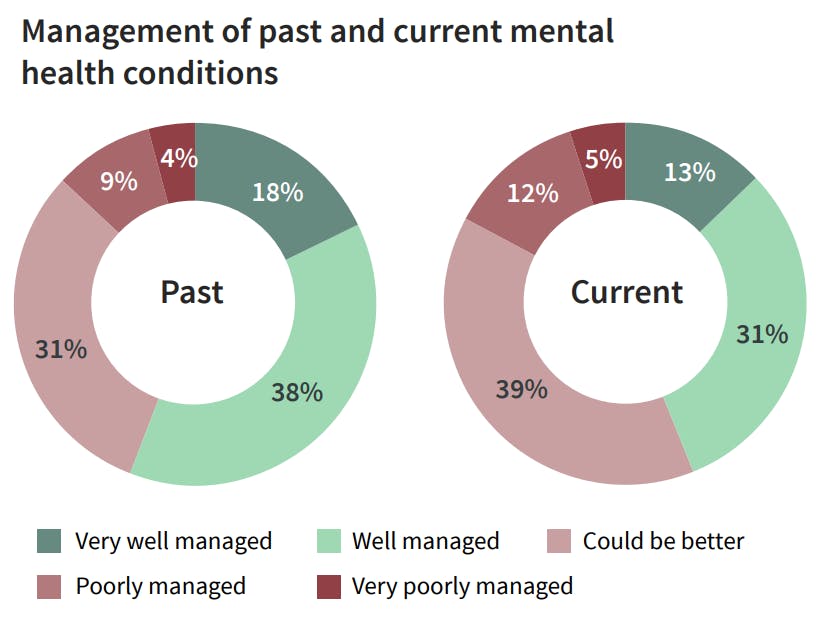
Over half of those with previous mental illness say it was well managed, but this figure falls below the halfway mark for those who are ill now.
This difference is possibly because it’s harder to draw conclusions for current illnesses as they are still being treated. The quality of care is vital in propelling those with mental illnesses toward a brighter future. Our study shows people whose illnesses are well managed stand a good chance of achieving the same levels of happiness as those who have never experienced mental illness.
[1] Please note that all references in this report to ‘China’ relate to mainland China, excluding Hong Kong.
[2] World Health Organization
[3] On the front line - the global economic impact of COVID-19 on women (AXA 2020)
[4] Ibid
[5] Comprehensive Psychiatry. Why women are less likely than men to commit suicide.
[6] American Journal of Men’s Health